Chondral Damage –
Articular Cartilage Damage
Knee Sports Injury
Chondral Damage - Articular Cartilage Damage
What is Hyaline articular cartilage ?
Hyaline articular cartilage is the connective tissue/material that covers the ends of the bone in all moving joints, this is a white /creamy coloured shiny and a very slippery tissue. It is a highly resilient structure; it resists compression and shear forces throughout life whilst allowing movement of the knee joint in many directions.
It can deteriorate over time to give rise to wear and tear (osteoarthritis). However, localized damage to this tissue can occur in young active adults as consequence of injury or at times no apparent cause and gives rise to a variety of symptoms. There are a number of well-recognised conditions, which cause chondral damage. Mr Aslam Mohammed treats these damaged areas in the hip and knee joint with joint preservation techniques where possible.
• Chondromalacia / Degenerative Chondrosis: Softening of the articular cartilage usually behind the kneecap, gives rise to a grating sensation.
• Osteochondritis Dissecans / Osteochondral Fracture: The cartilage breaks away with a piece of the bone and can float around the knee joint.
• Chondral Flaps: Cartilage separates from the bone and moves like a trap door with a hinge at one end.
Unfortunately hyaline articular cartilage tissue has no blood supply giving it very little or no capacity to heal and regenerate. The localised damage may be amenable various techniques to repair and help preserve the joint. In doing so it helps improve and restore function to the knee joint. The healing tissue that replaces the damaged area is called fibrocartilage almost like a scar, is not as resilient as normal articular cartilage to the loads placed upon it and it too can deteriorate over time and be damaged.
What are the symptoms?
Symptoms may start after an acute injury or activity and sometimes without any obvious cause or event.
Patients have pain, swelling of the knee joint with stiffness and limited movement, which are made worse with exercise and activity. They may have a sensation of catching, clicking, giving way and locking (getting stuck). Sometimes it may feel as if something is floating around in the knee joint.
What investigations are needed?
An X-ray is the initial investigation with different views being taken.
An MRI scan will look at the soft tissues and the articular cartilage in detail. It will also look at any abnormal reaction in the bone under the damaged articular cartilage.
How chondral injuries be managed?
Mr Aslam Mohammed has extensive experience in treating chondral injuries (articular cartilage). He aims to treat the focal defect with the most appropriate technique for the individual pathology and to return patients to near normal activity and lifestyle.
This decision is based on the patient’s activity level, age, cause, size and depth of the defects, presence of combined defects and other injuries to the knee joint.
Conservative measures may help with symptoms only and do not for restore the structural integrity of the articular cartilage and surgery may be required.
The purpose of surgical treatment is to improve symptoms and prevent progression of the degenerative changes, by achieving structural and biomechanical restoration and stabilisation of the articular cartilage.
Surgical treatment methods can be divided into:
• Arthroscopic lavage and debridement. This involves knee arthroscopy and debridement of the damaged articular cartilage (Chondroplasty), it removes the unstable fragments at the margins of the damaged cartilage that may be causing the symptoms and further damage to the joint. Basically smooth’s the roughened and damaged joint surface.
• Cell-based therapy with subchondral bone marrow stimulation using the technique of micro fracture. Knee arthroscopy is performed and pinholes are made into the exposed bone (micro fracture) 2-4 mm in depth and evenly spaced apart from each other.
This causes bleeding from the subchondral bone into the defect releasing mesenchymal stem cells, which then form a clot. These stem cells have the potential to change into fibrocartilage cells and chondrocytes and induce fibrocartilage or hyaline-like cartilage formation, so filling in the defect to help protect the joint and alleviate symptoms. This can be supplemented with a special membrane for the AMIC (Autologous Membrane Induced Chondrogenesis).
• Autologous Chondrocyte Implantation (ACI) is a two-stage procedure in which articular cartilage containing specialised cells (chondrocytes) is harvested from a non-weight bearing portion of the knee joint during keyhole surgery. These cells are then cultured (grown/ multiplied) in the laboratory. These cells then are implanted into the defect at a second operation requiring an open procedure.
• Tissue-based therapy osteochondral auto graft transplantation or osteochondral allograft transplantation. The advantages of these procedures are treating defects in one stage, promoting a more rapid return to daily living activities and sports with use of biomechanically healthy tissue and maintaining good results for a long-term due to the hyaline cartilage repair.
The advantages/disadvantages of each method are dependent on a number of factors which include: the size, site/location, depth of the lesion, and the patient’s age and activity level, compliance to post-operative rehabilitation and smoking status will all need to be taken into consideration.
What does cartilage surgery involve?
Mr Aslam Mohammed will discuss the details of what the surgical plan is with you before you make a decision. This firstly involves a knee arthroscopy and assessment of the knee and damaged articular surface. Dependent on the findings and discussions with you at the time of your consultation he will then proceed to perform the surgery.
What are the risks?
The risks of this type of surgery are relatively low but they always need to be taken into serious consideration before deciding to undergo surgery. Mr Aslam Mohammed will discuss these with in detail before you make decision to go ahead with surgery.
The following are potential risks:
• Thrombosis Blood Clots in the leg - DVT /Clots on the lung – PE
• Infection, Bleeding / Bruising, Swelling
• Wound pain and sensitivity, Nerve and vessel damage
• Graft harvest site pain and scarring
• Joint stiffness, On-going pain and discomfort
• Severe pain and stiffness and loss of use of your knee (complex regional pain syndrome), the cause is not known.
• Loss of confidence to play contact sport and do impact exercise
• Limited or no improvement in symptoms
• Graft cannot take or heal and deteriorate over time. It can also be damaged again during sport or after a fall.
• Over growth of the healing tissue (fibrocartilage) which may require further surgery
What are the outcomes?
Arthroscopic debridement can be helpful for preventing the progress of the delamination of the articular cartilage, but there is uncertainty over its effect on the long-term outcome (Chondroplasty).
A number of studies have shown that micro fracture can be helpful in improving overall symptoms of chondral defects, but the symptoms can progress over time. Poor clinical outcome are usually attributed to advanced age, large lesion size, and higher activity level. This is supported by Mr Aslam Mohammed’s experience over the last 25 years.
ACI shows good clinical outcomes for a longer period time in cases of focal cartilage defects, but the disadvantages include that it requires two separate procedures for chondrocyte collection and implantation.
Mr Aslam Mohammed has extensive experience in this technique and has participated in the ACTIVE multicentre study comparing various techniques with ACI.
The studies of the OATS (Osteochondral auto graft transplantation surgery also called mosaicplasty) show a positive outcome, many studies have shown that the technique was effective in 76-93% of the patients in achieving clinical improvement.
Overall despite all these treatment methods, deterioration in function and symptoms is expected over time of the articular cartilage and the onset of arthritis.
Examples of cartilage repair techniques
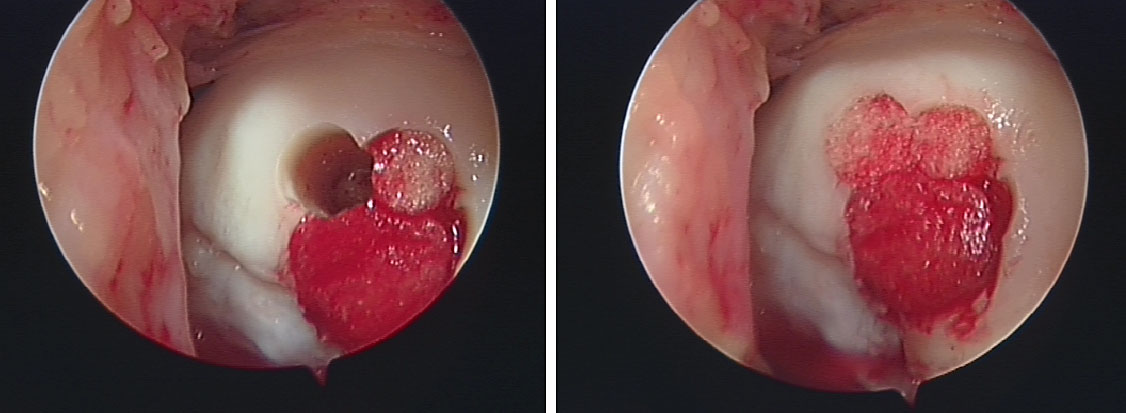 Defect in medial femoral condyle treated with OATS (Mosiacplasty) treated by Mr. Aslam Mohammed.
Defect in medial femoral condyle treated with OATS (Mosiacplasty) treated by Mr. Aslam Mohammed.

Micro fracture of the defect good bleeding seen into the defect which will form a fibrin clot then go onto form fibrocartilage, treated by Mr Aslam Mohammed.
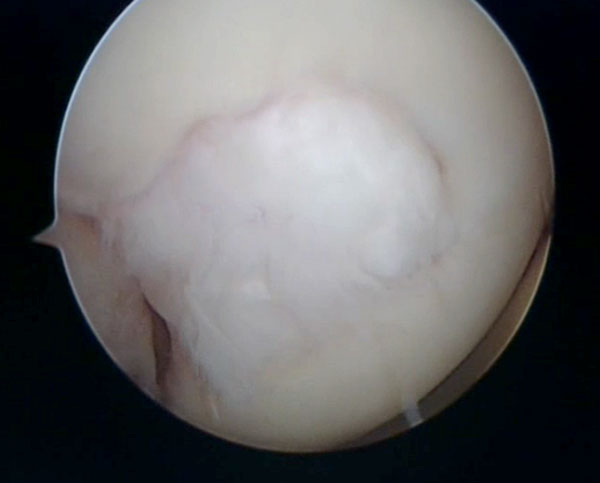 Defect treated with micro fracture seen at six month showing fibrocartilage has filled in the defect. treated by Mr. Aslam Mohammed.
Defect treated with micro fracture seen at six month showing fibrocartilage has filled in the defect. treated by Mr. Aslam Mohammed.
ACI (Autologous Chondrocyte Implantation)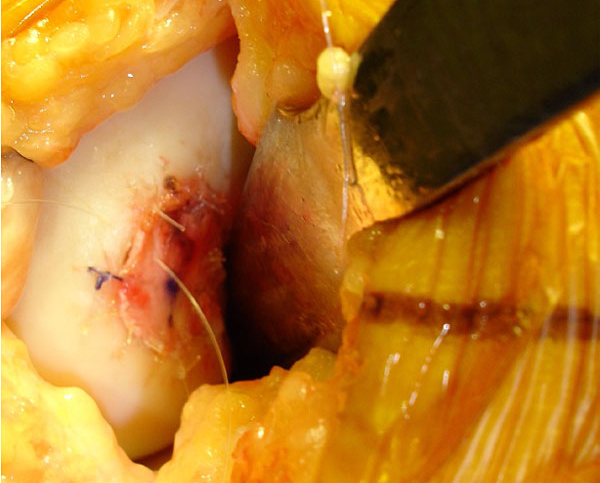
Mr. Aslam Mohammed performed this second stage of the ACI procedure on 19 years Netball player who had injured her left knee sustain a full thickness defect in the medial femoral condyle.
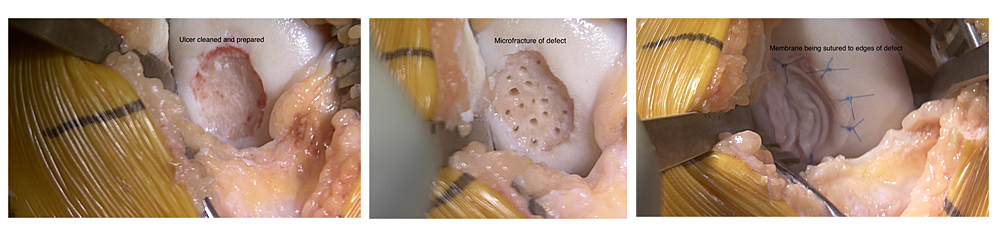
AMIC (Autologous Membrane Induced Chondrogenesis)
Case showing micro fracture of defect and a collagen membrane being sutured into place.
- Arthritis
- Knee Arthritis
- Knee Replacement
- Knee Sports Injury
- Knee Arthroscopy
- Knee Meniscus Tears
- Anterior Cruciate Ligament
- Chondral Injury / Cartilage Injury
North West Hip & Knee Clinics
Services provided:
• Keyhole (minimally invasive)
• Hip and Knee Surgery
• Hip and Knee Joint Replacement
• Hip and Knee Sports Injury
• Hip Arthroscopy, FAI and Labral Surgery
• Knee Arthroscopy - Meniscus surgery
• Knee Arthroscopy and ACL / PCL
• Ligament Reconstruction
• Biologics – PRP, Stem Cell
• Cartilage Regeneration
Mr Aslam Mohammed Consultant Hip and Knee Surgeon