Hip Arthritis
Hip Osteoarthritis (degenerative arthritis of the hip joint)
What is hip arthritis?
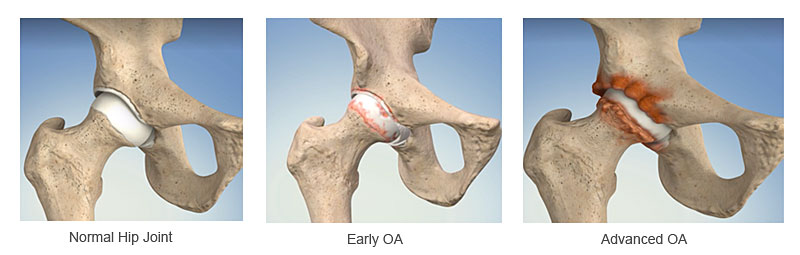
Arthritis means an inflamed painful joint. There are many different types of arthritis. The cause of osteoarthritis is multifactorial: genetic factors, poor development of the hip joint, childhood conditions, past injury or fractures and overloading the joint contribute to the development osteoarthritis.
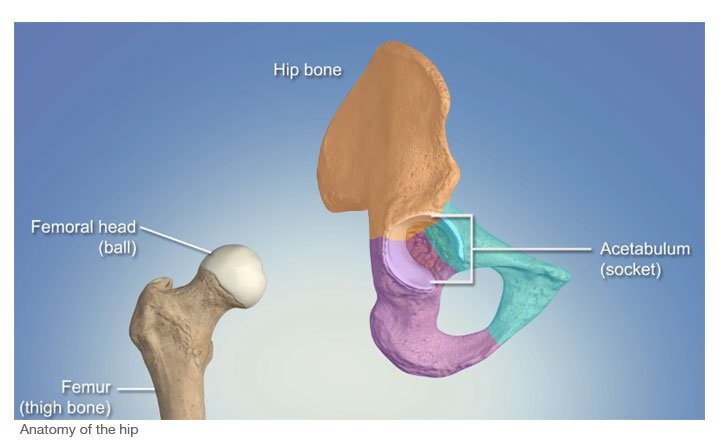
The most common type is the degenerative type, where the articular cartilage (the joint lining) wears away and the underlying bone is exposed and the gap between the two sides of the joint is reduced or completely lost. The anatomy of the hip is that it is a ball and socket joint and this becomes deformed, restricting the movement of the joint as well as causing pain and disability.
What are the symptoms of hip arthritis ?
Stiffness of the hip joint and reduced movement, both these come on gradually over many years.
Pain in the hip, buttock area, outer aspect of the hip going into the groin and sometimes pain is felt in the knee joint.
Pain may present at rest and made worse with activity.
There may be difficulty in:
• Walking, putting shoes and socks on, cutting toe nails and getting dressed.
• Getting in and out of the car, bath and climbing stairs and going down stairs.
• Overall activity and walking distance is reduced.
• You may feel the bones rubbing / grating together.
• Sleep can be disturbed and morning stiffness.
• Not being able to work.
What investigations are needed?
X rays of the hip joint
Additional investigations may be required in individual cases.
How can it be managed?
Initially conservative measure are utili sed to help with the pain and disability which include:
• Activity level and lifestyle can be modified
• Weight loss reduces load on the joint and can improve symptoms
• Diet, foods rich in Omega-3, may reduce inflammation or even the signs of arthritis.
• Physical therapy and regular non-impact exercise.
• Using a walking stick in the opposite hand
• Simple painkillers, anti–inflammatory medication and supplements can be of help.
• Hip joint injection with a steroid and local anaesthetic and or Hyaluronic acid (viscosupplements) an artificial synovial fluid these are carried out under X ray control. These may be of help, as well as confirming the pain is from the hip joint.
When all these interventions fail hip replacement may be the next option.
What does hip replacement surgery involve?
The hip replacement, replaces both the ball and socket of the hip joint.
Surgery is carried out most commonly under a spinal anaesthetic with sedation.
After surgery you be monitored and pain controlled. You will be taken back to the ward when stable and kept under observation.
You will mobilise the same day or certainly the next day with the physiotherapists and progress each day. You will be ready to go home usually day 2 or 3 after surgery, when you feel confident and able.
What are the risks?
All operations and intervention carry a risk. Measures are taken to reduce these risks and early mobilisation, antibiotics, compression stockings and blood thinning medication.
General risks:
• Anaesthetic
• Cardiac
• Respiratory
• Stroke
Risks specific to the operation:
• Infection – wound and deep joint
• Thrombosis – legs (DVT)
• Pulmonary embolism (PE)
• Dislocation of the hip replacement
• Leg length difference
• Intraoperative fracture
• Nerve and vessel damage
• Sensitive wounds
• Residual pain
• Wearing out of the bearing surface
• Implants becoming loose / Revision surgery
What are the outcomes of hip replacement?
It is generally acknowledged that the results of total hip replacement both functionally and in terms of longevity are very good and can life changing The majority of patients have improvement of pain and most patients get back to day-to-day activities. Many are able to return to work, exercise and play non-impact sports. Range of movement and function tend to be improved. Functional results are maintained over time. With present day materials, bearing surfaces and surgical techniques, there is a 90% chance that your hip will be functioning well at 10 years from the time of being replaced and 80% chance of it doing well at 20 years (See NJR)

1A. Osteoarthritis of Right Hip 60-year-old female (red arrow points to no joint space compared with the left hip which has early arthritis)

1B. Right Hip Replacement 12 months after surgery Patients doing very well and has returned to work with no pain and improved function.
North West Hip & Knee Clinic - Mr Aslam Mohammed
GC 68 year old male presented to Mr Aslam Mohammed with right hip pain and leg shortening. Disabling symptoms and stiffness.
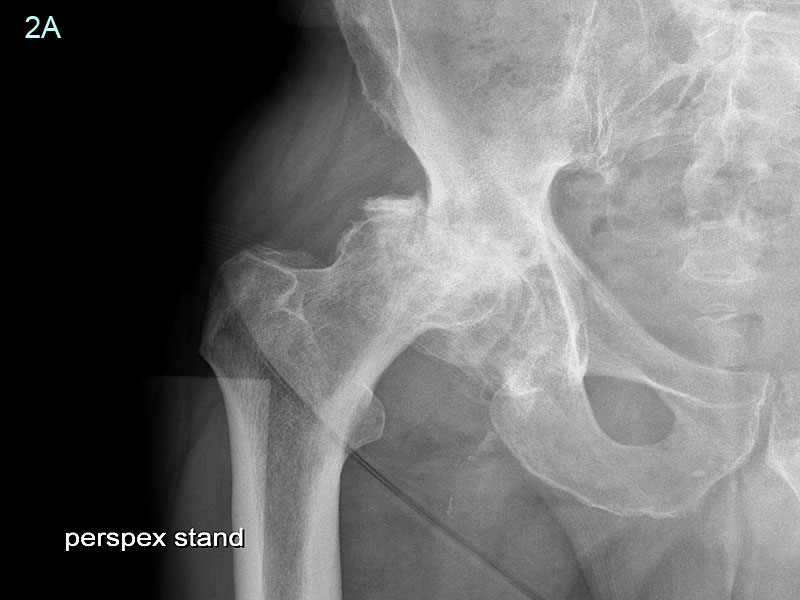
2A. GC Radiographs show collapse of the femoral head (Ball) and migration of the hip out of the acetabulum (Socket) causing damage to it. Requiring the need to put a bone graft in the acetabulum to reconstruct the socket.

2B. GC Postoperative radiographs showing the hip replacement with reconstruction of the socket using bone graft fixed with screws. Patient reported no pain and near normal function six months after surgery.
MC 54 year-old male HGV diver presented to Mr Aslam Mohammed with disabling bilateral hip pain and extreme stiffness, no longer able to work, this had progressed over a number of years.

3A. MC Radiographs showing advanced arthritis of both hips and the femoral heads have been destroyed. Both hips required replacement. This was undertaken at one operation where both hips were replaced.

3B.
MC Post operative radiographs at 9 years after replacement of both hips using uncemented hips. He had been able to return to work and lead a normal life style.
- Arthritis
- Hip Arthritis
- Hip Replacement
- Hip Sports Injury
- Hip Arthroscopy
- Hip Labrum Tears
- Hip Femoro Acetabular Impingement
- Psoas Tendon Snapping
- Soft Tissue Hip Problems
- History Of Hip Replacement
North West Hip & Knee Clinics
Services provided:
• Keyhole (minimally invasive)
• Hip and Knee Surgery
• Hip and Knee Joint Replacement
• Hip and Knee Sports Injury
• Hip Arthroscopy, FAI and labral surgery
• Knee Arthroscopy - Meniscus surgery
• Knee Arthroscopy - ACL / PCL
• Ligament Reconstruction
• Biologics – PRP, Stem Cell
• Cartilage Regeneration
Mr Aslam Mohammed Consultant Hip and Knee Surgeon